What is DNA Testing for Health Optimization?
DNA testing for health represents the frontier of personalized medicine, moving healthcare from one-size-fits-all approaches to individualized strategies based on your unique genetic blueprint. While traditional medicine treats populations similarly, genetic health testing reveals how your specific DNA influences disease risk, medication response, nutritional needs, fitness potential, and aging—enabling truly personalized health optimization.
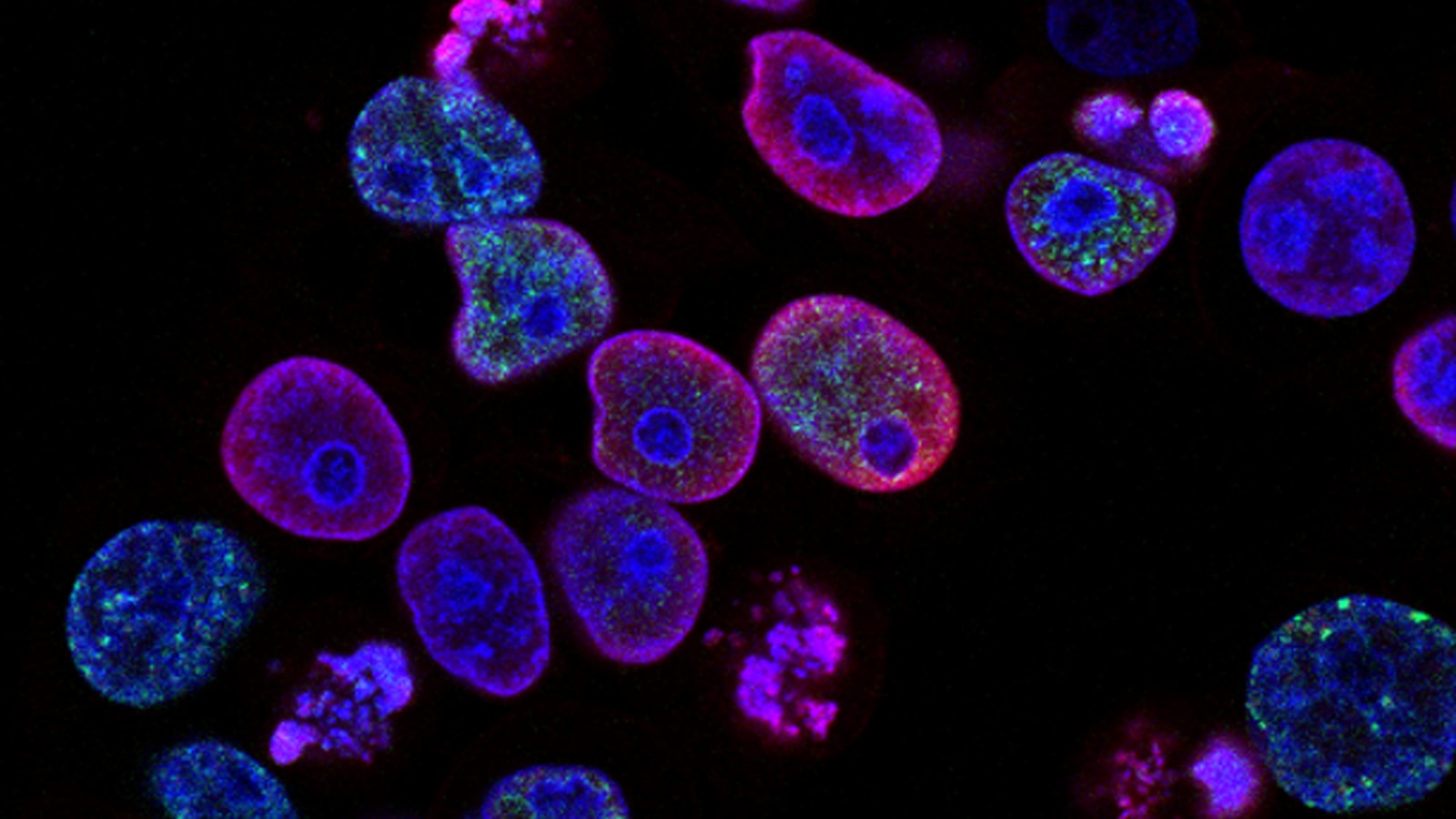
Your DNA contains approximately 20,000-25,000 genes encoding instructions for every biological process in your body. Small variations in these genes—called single nucleotide polymorphisms (SNPs)—create the genetic diversity making each person unique. These variations influence everything from how efficiently you metabolize caffeine to your risk of developing Alzheimer's disease decades from now.
Modern genetic testing in the UK has evolved dramatically from rare medical applications to accessible consumer services offering comprehensive health insights. Whether through NHS genetic services for clinical conditions or private testing for health optimization, DNA analysis now provides actionable information for preventing disease, personalizing nutrition and fitness, optimizing medication selection, and understanding your body's unique characteristics.
Types of DNA Health Tests
Whole Genome Sequencing
Whole Genome Sequencing (WGS) analyzes all 3 billion base pairs in your DNA, providing the most comprehensive genetic information possible. This approach sequences your entire genome, identifying virtually all genetic variants you carry, including rare mutations not covered by targeted testing.
WGS applications include diagnosing rare genetic disorders, identifying cancer-related mutations, comprehensive disease risk assessment, and research into novel genetic associations. The cost has decreased dramatically—from millions of pounds in 2003 to under £1,000 today—making comprehensive genetic analysis increasingly accessible.
However, WGS generates massive data requiring expert interpretation. Most genetic variants have unknown clinical significance, creating interpretive challenges. WGS is most valuable when comprehensive genetic information is needed, such as diagnosing complex undiagnosed conditions or for individuals with strong family history of multiple diseases.
Targeted SNP Genotyping
SNP genotyping (single nucleotide polymorphism testing) analyzes specific genetic variants known to influence health. Rather than sequencing your entire genome, these tests examine hundreds of thousands to millions of predetermined genetic locations associated with disease risk, traits, and medication response.
This approach offers excellent cost-effectiveness—comprehensive SNP panels cost £150-400 versus £800-2,000 for WGS—while providing actionable insights for most health optimization purposes. SNP testing covers the genetic variants with established clinical significance, focusing on information you can actually use.
Most direct-to-consumer genetic health tests use SNP genotyping, analyzing 500,000 to 700,000+ SNPs covering: disease predisposition genes, pharmacogenomic variants affecting medication response, nutrigenomics markers influencing nutrition, fitness and performance genetics, and traits affecting weight, sleep, and aging.
Clinical Genetic Testing
Clinical genetic testing targets specific genes or conditions when medical indication exists. This includes diagnostic testing (identifying genetic cause of symptoms), predictive testing (assessing disease risk before symptoms appear), carrier screening (determining if you carry recessive disease genes), and prenatal/newborn testing.
Clinical testing uses medical-grade laboratories meeting stringent quality standards, with results interpreted by genetic counselors or medical geneticists. In the UK, NHS provides clinical genetic testing when family history, symptoms, or medical circumstances warrant investigation—typically for cancer predisposition (BRCA1/2), cardiac conditions, rare diseases, or reproductive planning.
Private clinical genetic testing costs £300-800+ depending on genes analyzed but provides the highest quality interpretation with genetic counseling support, essential when testing for serious hereditary conditions.
Nutrigenomics Testing
Nutrigenomics examines genetic variants influencing nutrient metabolism, food sensitivities, and dietary response. This specialized testing reveals how your genetics affect vitamin and mineral needs, macronutrient metabolism, food intolerances and sensitivities, optimal diet type, and supplement requirements.
Key nutrigenomics insights include: caffeine metabolism (CYP1A2 gene determines fast or slow caffeine clearance), carbohydrate sensitivity (variants affecting insulin response and carbohydrate tolerance), fat metabolism (genes influencing response to dietary fats), vitamin D requirements (genetic factors affecting vitamin D synthesis and metabolism), folate metabolism (MTHFR variants requiring methylated B-vitamins), and lactose tolerance (LCT gene determines adult lactose digestion capacity).
Research published in the Journal of Nutrigenetics and Nutrigenomics (2022) demonstrates that genetics-based dietary recommendations improve outcomes compared to generic dietary advice, with participants following nutrigenomics-guided nutrition achieving better weight loss, metabolic markers, and long-term adherence.
Pharmacogenomics Testing
Pharmacogenomic testing analyzes genes affecting drug metabolism, response, and adverse reaction risk. This testing identifies genetic variants in drug-metabolizing enzymes, drug targets, and drug transporters—information predicting medication effectiveness and optimal dosing for your unique genetics.
Critical pharmacogenomic genes include: CYP450 enzymes (metabolize over 70% of commonly prescribed medications), TPMT and NUDT15 (affect immunosuppressant metabolism), HLA genes (predict severe drug reactions), VKORC1 and CYP2C9 (guide warfarin dosing), and CYP2D6 and CYP2C19 (affect antidepressant and pain medication response).
Pharmacogenomic testing prevents dangerous trial-and-error prescribing, particularly for psychiatric medications where finding effective treatment often requires multiple attempts. Knowing your medication metabolism profile before starting treatment saves time, prevents adverse reactions, and identifies optimal medications faster.
What Your DNA Reveals About Your Health
Disease Risk Assessment
Genetic testing identifies increased or decreased risk for numerous common diseases, enabling proactive prevention strategies. Unlike simple Mendelian disorders caused by single-gene mutations, most common diseases result from complex interactions between multiple genes and environmental factors.
Cardiovascular Disease Risk: Genetic variants affecting cholesterol metabolism (APOE, LDLR, PCSK9), blood pressure regulation, clotting factors, and inflammation influence heart disease and stroke risk. Polygenic risk scores aggregate effects of dozens or hundreds of variants, estimating your cardiovascular risk independent of traditional risk factors. High genetic cardiovascular risk justifies more aggressive prevention—earlier and more frequent screening, stricter lipid targets, and intensive lifestyle modification.
Type 2 Diabetes Risk: Variants in TCF7L2, PPARG, KCNJ11, and other genes affect insulin production, insulin sensitivity, and beta-cell function. Genetic diabetes risk assessment combined with biomarkers (fasting glucose, HbA1c, insulin) provides superior risk prediction compared to either alone, enabling targeted prevention through diet, exercise, and potentially metformin for high-risk individuals.
Cancer Predisposition: While most cancers aren't strongly genetic, certain variants dramatically increase risk. BRCA1 and BRCA2 mutations increase breast and ovarian cancer risk up to 80%, warranting enhanced surveillance or preventive surgery. Lynch syndrome genes (MLH1, MSH2, MSH6, PMS2) increase colorectal and other cancer risks. TP53 mutations (Li-Fraumeni syndrome) elevate risk for multiple cancer types. Genetic cancer risk assessment guides screening frequency and preventive strategies.
Alzheimer's and Neurodegenerative Disease: The APOE ε4 allele increases Alzheimer's risk approximately 3-fold for one copy, 12-fold for two copies, though many APOE ε4 carriers never develop dementia. Other variants affect risk for Parkinson's disease, ALS, and frontotemporal dementia. While no cure exists yet, knowing neurodegenerative risk enables lifestyle optimization (exercise, Mediterranean diet, cognitive engagement, sleep, stress management) proven to reduce risk.
Fitness and Performance Genetics
Your genetic blueprint significantly influences athletic potential, training response, injury risk, and optimal exercise programming. Sports genetics testing reveals actionable insights for performance optimization.
Muscle Fiber Type: The ACTN3 gene determines presence of alpha-actinin-3 protein in fast-twitch muscle fibers. The R577X variant creates "functional" (RR or RX genotypes with fast-twitch capacity) versus "deficient" (XX genotype lacking fast-twitch protein) variants. XX individuals tend toward endurance performance, while RR individuals excel in power and strength. This information guides training focus—XX genotypes benefit from power training to compensate for genetic endurance bias, while RR genotypes may need more endurance work.
VO2 Max Trainability: Variants in genes like PPARGC1A, VEGF, and ACE affect cardiovascular adaptability to training. Some individuals are "high responders" gaining substantial aerobic capacity from training, while "low responders" show minimal VO2 max improvements despite training. Understanding your responder status optimizes training volume and intensity.
Recovery Capacity: Genetic variants influence inflammation, oxidative stress response, and tissue repair speed. IL6, TNF-alpha, and SOD2 variants affect post-exercise recovery time, informing optimal training frequency and recovery protocols.
Injury Risk: Collagen genes (COL1A1, COL5A1) affect tendon and ligament strength. Certain variants increase ACL tear, Achilles tendon injury, and stress fracture risk. Athletes with high-risk variants benefit from targeted injury prevention—additional strengthening work, careful load management, and appropriate recovery time.
Aging and Longevity Genetics
Genetic variants influence biological aging rate, cellular senescence, telomere maintenance, and longevity. While lifestyle dominates aging outcomes, genetics contribute approximately 25-30% of longevity variance.
Telomere Biology: Telomeres—protective caps on chromosome ends—shorten with each cell division, eventually triggering cellular senescence. Variants in TERT (telomerase reverse transcriptase) and other telomere maintenance genes affect baseline telomere length and attrition rate. While you cannot change these variants, knowing accelerated telomere shortening risk justifies intensive lifestyle optimization (exercise, stress management, sleep) proven to slow telomere attrition.
Sirtuins and NAD+ Metabolism: SIRT1 and other sirtuin genes regulate metabolism, inflammation, and cellular stress resistance—processes central to aging. Variants affecting sirtuin expression or activity may influence response to caloric restriction, resveratrol, and NAD+ precursors like NMN or NR.
Growth Hormone and IGF-1: GH1 and IGF1 variants affect growth hormone and insulin-like growth factor 1 levels. Paradoxically, lower IGF-1 associates with increased longevity in some studies, possibly through reduced cancer risk and enhanced cellular stress resistance. Understanding your genetic IGF-1 tendencies informs protein intake optimization and perspectives on growth factor modulation.
Inflammation and Immune Function: Variants in IL6, TNF-alpha, CRP, and other inflammatory genes create "high inflammatory responder" versus "low inflammatory responder" profiles. High inflammatory responders benefit especially from anti-inflammatory nutrition, omega-3 supplementation, and inflammation-dampening lifestyle practices.
Nutrigenomics: Personalized Nutrition Based on DNA
Macronutrient Metabolism and Diet Optimization
Genetic variants significantly influence how your body processes carbohydrates, fats, and proteins, suggesting optimal macronutrient ratios for weight management, energy, and health.
Carbohydrate Sensitivity: Variants in TCF7L2, PPARG, IRS1, and other genes affect insulin secretion, insulin sensitivity, and glucose metabolism. "Carbohydrate sensitive" genotypes show greater blood sugar and insulin response to carbohydrate intake, benefiting from lower-carbohydrate approaches. Conversely, some genotypes maintain excellent glucose control on higher-carbohydrate diets. Matching carbohydrate intake to genetic tolerance improves metabolic health.
Fat Metabolism: APOA2, PPARG, and FABP2 variants influence fat absorption, metabolism, and body composition response to dietary fat. Certain genotypes gain more weight on high-fat diets, while others maintain lean mass better with higher fat intake. The APOE gene also affects cholesterol response to dietary fat—APOE ε4 carriers often show greater LDL increases from saturated fat, warranting stricter saturated fat limitation.
Protein Needs: While less genetically variable than carbohydrate and fat metabolism, variants affecting mTOR signaling, amino acid metabolism, and muscle protein synthesis influence optimal protein intake. Athletes with "high protein need" genetics may require 2.0-2.5 g/kg versus 1.6-2.0 g/kg for optimal muscle maintenance and recovery.
Vitamin and Mineral Genetics
Vitamin D Metabolism: VDR (vitamin D receptor), CYP2R1, and GC (vitamin D binding protein) variants affect vitamin D synthesis, activation, transport, and receptor binding. Some genotypes require higher vitamin D intake to achieve optimal blood levels (75-125 nmol/L), while others efficiently maintain vitamin D status with minimal supplementation. Combining genetic testing with 25(OH)D blood testing optimizes supplementation.
B-Vitamin Metabolism: The MTHFR C677T polymorphism reduces activity of the methylenetetrahydrofolate reductase enzyme, impairing folate metabolism and homocysteine clearance. Approximately 40-50% of people carry at least one T allele. TT homozygotes (10-15% of population) have significantly reduced enzyme activity, increasing homocysteine and cardiovascular risk. These individuals benefit from methylated B-vitamins (methylfolate, methylcobalamin) rather than standard folic acid supplements.
Iron Regulation: HFE gene mutations cause hereditary hemochromatosis, where excessive iron absorption leads to iron overload and organ damage. H63D and C282Y variants are common—C282Y homozygotes (1 in 300 people) require monitoring and sometimes phlebotomy. Even heterozygotes may accumulate excess iron, warranting ferritin monitoring and avoiding unnecessary iron supplementation.
Omega-3 Fatty Acids: FADS1 and FADS2 genes encode enzymes converting plant-based omega-3 (ALA) to EPA and DHA. Poor converter genotypes struggle to synthesize EPA/DHA from flaxseed or walnuts, requiring direct EPA/DHA from fish or algae supplements. Approximately 25% of people are poor converters.
Food Sensitivities and Intolerances
Lactose Intolerance: The LCT gene regulates lactase persistence—the ability to digest lactose (milk sugar) into adulthood. The C/T-13910 variant determines lactose tolerance. CC genotype creates lactase non-persistence (lactose intolerance) in most adults worldwide, while CT and TT genotypes maintain lactase activity. Genetic testing definitively identifies lactose intolerance genetics, though clinical symptoms and hydrogen breath testing confirm functional intolerance.
Gluten Sensitivity and Celiac Risk: HLA-DQ2 and HLA-DQ8 variants are necessary (but not sufficient) for celiac disease. Approximately 30-40% of people carry these variants, but only 1% develop celiac. Absence of DQ2/DQ8 virtually rules out celiac disease risk. Carrying these variants doesn't mean you should avoid gluten, but justifies testing if digestive symptoms appear.
Caffeine Metabolism: CYP1A2 variants create "fast" or "slow" caffeine metabolizers. Fast metabolizers (AA genotype) clear caffeine quickly, tolerating multiple cups daily without sleep disruption or anxiety. Slow metabolizers (AC or CC genotype) experience prolonged caffeine effects, requiring limitation to morning consumption to avoid sleep interference. Slow metabolizers also show increased cardiovascular event risk from high caffeine intake in some studies.
Pharmacogenomics: Medication Response and Safety
Cytochrome P450 Enzymes
The CYP450 enzyme family metabolizes over 70% of prescription medications. Genetic variants create "poor metabolizers," "intermediate metabolizers," "normal metabolizers," and "ultra-rapid metabolizers"—dramatically affecting drug blood levels, efficacy, and side effect risk.
CYP2D6: This enzyme metabolizes antidepressants (SSRIs, tricyclics), pain medications (codeine, tramadol, oxycodone), antipsychotics, and beta-blockers. Poor metabolizers experience high drug levels and increased side effects from standard doses. Paradoxically, codeine is ineffective in poor metabolizers because CYP2D6 converts codeine to morphine—without this conversion, codeine provides no pain relief. Ultra-rapid metabolizers may need higher doses of standard medications but experience dangerous morphine levels from codeine.
CYP2C19: Critical for metabolizing proton pump inhibitors (PPIs), antidepressants (SSRIs), clopidogrel (blood thinner), and benzodiazepines. CYP2C19 poor metabolizers show excellent response to PPIs but increased side effects from antidepressants. Most concerning, clopidogrel requires CYP2C19 activation—poor metabolizers have reduced antiplatelet effect, increasing cardiovascular event risk after stenting. Alternative blood thinners should be considered.
CYP2C9: Metabolizes warfarin, NSAIDs, phenytoin, and some diabetes medications. Combined CYP2C9 and VKORC1 genetic testing optimizes warfarin dosing, reducing dangerous bleeding risk and time to therapeutic anticoagulation.
Medication-Specific Pharmacogenomics
Psychiatric Medications: Finding effective psychiatric medication often requires trying multiple drugs—a frustrating trial-and-error process. Pharmacogenomic testing analyzing CYP2D6, CYP2C19, and other relevant genes identifies medications most likely to work for your genetics while avoiding those likely to cause side effects. This approach reduces time to effective treatment from months to weeks, preventing medication-induced deterioration and improving outcomes.
Pain Management: Opioid response varies dramatically by genetics. CYP2D6 affects codeine, tramadol, and oxycodone metabolism. OPRM1 variants influence opioid receptor sensitivity. COMT variants affect pain perception and opioid requirements. Pharmacogenomic testing guides safer, more effective pain management—critical given opioid risks.
Statin Response: SLCO1B1 variants affect statin uptake into liver cells. Certain genotypes show increased myopathy (muscle pain) risk from simvastatin and atorvastatin. Alternative statins (pravastatin, rosuvastatin) or lower doses prevent muscle problems while maintaining cholesterol control.
DNA Testing Options in the UK
NHS Genetic Testing Services
NHS provides genetic testing and counseling when medical indication exists—typically strong family history of genetic conditions, unexplained symptoms suggesting genetic cause, cancer predisposition assessment, or reproductive planning.
NHS genetic services include: diagnostic testing for rare diseases and genetic conditions, predictive testing for cancer predisposition (BRCA, Lynch syndrome), carrier screening before pregnancy, prenatal testing when indicated, and genetic counseling explaining results and implications.
Referral requires GP or specialist assessment. Testing is free but limited to clinically indicated circumstances. Results are medical-grade with genetic counselor interpretation—essential for serious hereditary conditions.
Private DNA Health Testing
Private genetic testing offers comprehensive health insights beyond NHS criteria, enabling health optimization rather than just disease diagnosis. Direct-to-consumer testing provides results without GP referral, though professional interpretation is valuable.
Leading UK Providers: 23andMe Health + Ancestry (£149-199), MyHeritage DNA Health (£140), Living DNA Wellbeing (£99-149), and specialized providers like Muhdo (fitness and epigenetics, £159) and DNAfit (sports and nutrition, £199). Clinical-grade testing through providers like Genomics England and private genetic counseling services costs £300-800+ but offers superior interpretation.
Comprehensive Health Panels: Best value testing covers disease risk, nutrigenomics, pharmacogenomics, fitness genetics, and traits in single comprehensive panel (£200-400). While more expensive than basic ancestry tests, comprehensive panels provide actionable insights across all health domains.
Choosing the Right DNA Test
For general health optimization and personalized nutrition, comprehensive SNP panels from reputable providers offer excellent value. Look for tests analyzing 500,000+ SNPs, evidence-based interpretation, privacy protection, and option to download raw data.
For serious hereditary disease concerns (cancer predisposition, cardiac conditions), choose clinical-grade testing with genetic counseling. NHS services are appropriate when criteria are met; private clinical testing costs more but provides access without referral delay.
For medication optimization, specialized pharmacogenomic panels focusing on drug metabolism genes provide most relevant information. Some comprehensive health tests include pharmacogenomics; ensure CYP2D6, CYP2C19, CYP2C9, and VKORC1 are covered.
Understanding Your DNA Test Results
Interpreting Genetic Risk
Genetic risk is probability, not certainty. "High genetic risk" means increased likelihood compared to average population risk—not that disease is inevitable. Conversely, "low genetic risk" doesn't guarantee disease prevention.
Understanding relative versus absolute risk is critical. If a genetic variant doubles your risk (relative risk 2.0) but baseline risk is 0.5%, your absolute risk increases to only 1%—still low despite "doubled risk." Context matters enormously.
Polygenic risk scores aggregate effects of multiple genetic variants, providing more accurate risk assessment than single genes. These scores place you in risk percentiles—being in the 90th percentile means 90% of people have lower genetic risk than you, justifying more aggressive prevention.
Limitations and Considerations
Current genetic testing has important limitations. We don't understand effects of all genetic variants—many results will show "variants of uncertain significance." Genetic testing reveals what we know today; understanding improves as research advances.
Most common diseases result from gene-environment interactions. Your genetic predisposition interacts with lifestyle, environment, and chance. Even high genetic risk can often be mitigated through optimal lifestyle—genetics loads the gun, but lifestyle pulls the trigger.
Genetic testing cannot predict everything. Complex traits like intelligence, personality, and many aspects of health involve thousands of genetic variants plus environmental factors—too complex for accurate prediction from current genetic tests.
Clinical Evidence and Research
Research published in Nature Reviews Genetics (2023) demonstrates that personalized medicine approaches based on genetic testing improve outcomes across multiple domains. Pharmacogenomic testing reduces adverse drug reactions by 30-50% and improves time to effective psychiatric medication treatment by 40-60%.
Studies in Annual Review of Genomics and Human Genetics (2023) show that genetic risk assessment combined with biomarker monitoring enables earlier disease detection and more effective prevention compared to standard approaches. High-risk individuals benefit most from intensive screening and prevention.
Nutrigenomics research published in the Journal of Nutrigenetics and Nutrigenomics (2022) demonstrates that genetics-based dietary recommendations produce better weight loss, metabolic health improvements, and long-term adherence compared to generic dietary advice.
Pharmacogenomics studies in Science (2022) confirm that CYP450 genetic testing significantly reduces trial-and-error prescribing for antidepressants, pain medications, and cardiovascular drugs, improving outcomes while reducing adverse effects and healthcare costs.
Getting Started with DNA Health Testing
Your First DNA Test
If you've never had genetic testing, start with comprehensive health panel covering disease risk, nutrigenomics, fitness, and ideally pharmacogenomics. This establishes your genetic baseline and identifies priorities for personalized optimization.
Testing process is simple: order online, receive saliva collection kit, provide saliva sample (no blood draw needed), mail sample to laboratory, and receive results in 2-6 weeks. Most providers offer online results portals with detailed reports.
Consider professional interpretation—genetic counselors, functional medicine practitioners, or providers offering genetic counseling services help translate results into actionable strategies. Raw genetic data is valuable but requires expertise to interpret optimally.
Implementing Genetic Insights
After receiving genetic results, prioritize actionable findings: high disease risks warranting enhanced screening or prevention, nutrigenomics insights enabling dietary personalization, pharmacogenomic information for current or future medications, and fitness genetics optimizing training approaches.
Combine genetic testing with biomarker monitoring. DNA reveals predispositions; blood biomarkers show current status. Together, they enable truly personalized optimization—genetics guide strategy; biomarkers measure effectiveness.
Share relevant genetic information with healthcare providers, particularly pharmacogenomic results affecting medication selection. While some providers remain unfamiliar with genetic testing, increasing numbers integrate genetic information into clinical care.
Protecting Your Genetic Privacy
Choose providers with strong privacy policies and data security. Look for: GDPR compliance (required in UK), data encryption, clear policies on data sharing and third-party access, and ability to download and delete your data.
Consider implications before sharing genetic data with research databases. While contributing to research benefits society, understand privacy tradeoffs. Anonymous genetic data can potentially be re-identified, particularly if multiple databases are cross-referenced.
Be aware of potential insurance and employment implications. UK law prohibits genetic discrimination in most contexts, but understand your rights and provider policies before testing for serious hereditary conditions outside NHS services.